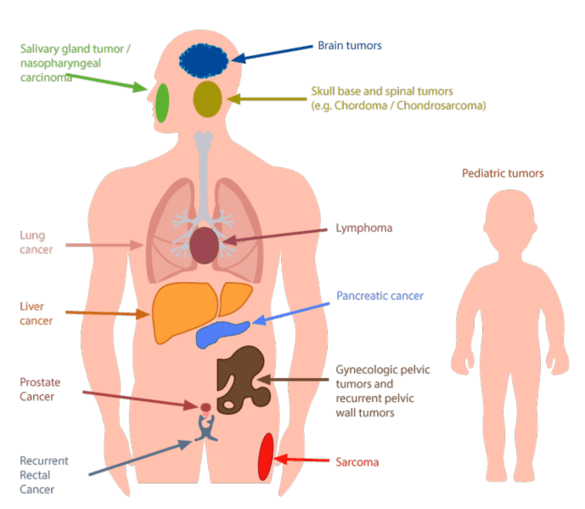
Proton therapy is preferred especially for specific cancer types in children, since surrounding healthy tissue is maximally spared. Thus, growth and development deficits as well as the development of further tumors can be prevented.
In infants and small children, depending on the age, radiation is only possible under anesthesia (twilight sleep / no general anesthesia) because they must remain completely still. Even with positioning assistance, this can often still not be obtained with children. Daily anesthesia is performed by experienced anesthesiologists and with the least possible amount of medications given. Treatment takes place in close collaboration with the Department of Pediatric Oncology, Hematology, and Immunology. Because the children may not have breakfast, these treatments are always performed first in the morning. Children like to bring a stuffed animal for comforting.